by J. Dean and P. Kendall* (8/12)
Quick Facts…
- During pregnancy, changes in hormones cause a woman’s immune system to become suppressed, so that it is harder to fight off infections.
- Pregnant women are at increased risk for some types of food borne illness.
- Some food borne illnesses can cause a woman to have a miscarriage, stillbirth or serious health problems for the baby after birth.
- Pathogens are organisms (bacteria, virus, parasite) that can cause illness in humans.
Pregnancy is an exciting, yet critical time in a woman’s life. Because a mother’s health behaviors have direct effects on the health of her baby, expectant mothers receive a lot of health information. Along with nutrition concerns, a growing topic of importance is food safety during pregnancy. Pregnant women are at increased risk for getting some foodborne infections because of the hormonal changes that occur during pregnancy. While such changes are necessary for survival of the fetus, they also suppress the mother’s immune system, thereby increasing the chance of infection from certain foodborne pathogens.
Examples of pathogens of special concern to pregnant women are Listeria monocytogenes, Toxoplasma gondii, Brucella species, Salmonella species and Campylobacter jejuni. Certain organisms can cross the placenta and increase the fetus’s risk of becoming infected. Infection can result in miscarriage, stillbirth, premature labor or severe complications for the baby. Certain organisms, including Listeria monocytogenes, Toxoplasma gondii, Salmonella typhi and Campylobacter jejuni, can have adverse consequences for the fetus if they cross the placenta.
Listeriosis
Listeriosis is a form of infection that may result when foods containing the bacteria Listeria monocytogenes are consumed. L. monocytogenes is widely distributed in nature and is found in soil, ground water, plants and animals. L. monocytogenes is often carried by humans and animals, and has the ability to survive unfavorable conditions, including refrigeration temperatures, food preservatives (salt), and conditions with little or no oxygen. It is, however, easily destroyed by cooking.
Infection from L. monocytogenes typically occurs in individuals with a weakened immune system, including pregnant women. There is an estimated 14-fold increase in the incidence of listeriosis among pregnant women compared to non-pregnant adults. Pregnant women make up 17 percent of all cases of listeriosis. Once in the bloodstream, Listeria bacteria can travel to any site, but seem to prefer the central nervous system and the placenta. The fetus is unusually prone to infection from L. monocytogenes, which can lead to a miscarriage, stillbirth, or infection of the neonate and health problems following birth.
Gastrointestinal symptoms may appear within 2 to 3 days of exposure. If the body does not clear itself of the pathogen and the infection becomes invasive, symptoms such as fever, chills, headache, muscle aches and back aches may develop in 11 to 70 days after exposure. A blood test can determine if symptoms are caused by Listeria infection and if confirmed, the patient can then be treated with antibiotics.
Foods typically associated with listeriosis include refrigerated ready-to-eat perishable foods with a long shelf life that are eaten without further cooking. Outbreaks have involved foods such as coleslaw, Mexican-style soft cheeses, milk, pâté, pork tongue, cantaloupe, hot dogs, processed meats and deli salads. Examples of foods that may harbor this pathogen include unpasteurized milk, raw milk products, raw and smoked seafood, and any refrigerated ready-to-eat processed foods, such as hot dogs, luncheon meats or deli meats, that have not been heated to proper temperatures before serving.
To avoid infection from L. monocytogenes, pregnant women are advised to practice safe food handling procedures, such as storing all perishable foods between 35 and 40 degrees F and using perishable refrigerated ready-to-eat foods as soon as possible. If a potentially hazardous perishable food cannot be eaten within four days, it is best to freeze or discard it. Kitchen surfaces, cutting boards and utensils should be washed before and after food preparation (especially after contact with raw meat or poultry). Pregnant women are advised to avoid eating soft cheeses made with raw milk (e.g., Feta, Brie, Camembert, blue-veined cheeses, queso fresco, queso blanco and Panela), unpasteurized milk and uncooked foods made with raw milk, raw or undercooked seafood, refrigerated smoked or precooked seafood, deli seafood salads, and hot dogs, luncheon meats, deli meats and pâté unless reheated to steaming hot before serving or reformulated to prevent Listeria. Leftover foods should be reheated to 165 degrees F before eating.
Toxoplasmosis
Toxoplasmosis, the infection caused by the parasite Toxoplasma gondii, can be passed to humans by water, dust, soil, or through eating contaminated foods. Cats are the main host for T. gondii, and the only host where the parasite can complete its life cycle. T. gondii may be carried in the fur or feces of cats and then passed to other animals and people. If an animal becomes infected and its meat is then eaten raw or undercooked, the parasite is passed to the human or animal that consumes the meat.
It is estimated that 1.5 million people in the U.S. become infected with T. gondii each year. Most individuals do not experience recognizable symptoms, and will develop a protective resistance to the parasite. However, if a woman not previously exposed to T. gondii first acquires the parasite a few months before or during pregnancy, she may pass the organism to the fetus. This could result in stillbirth, early prenatal death, or serious health problems for the baby after birth such as eye or brain damage. Symptoms in the baby may not be visible at birth, but can appear months or even years later.
If symptoms of infection with T. gondii do appear in the pregnant woman, they usually appear about 10 days after exposure to the parasite and include a low grade fever with rash, muscle aches, headache and possibly swelling of the lymph nodes. Infection may be confirmed by a blood test and treated with antibiotics. Prompt treatment of the mother with antibiotics reduces the risk of passing the parasite to the fetus, but cannot change the course of the disease once the fetus has been exposed.
Toxoplasmosis most often results from eating raw or undercooked meat, eating unwashed fruits and vegetables, cleaning a cat litter box or handling contaminated soil.
To avoid infection from T. gondii it is important that pregnant women practice safe food handling procedures such as washing all surfaces, cutting boards and utensils with hot, soapy water, especially those that come in contact with raw meat. Pregnant women should wash hands often, especially after handling animals or working in the garden, avoid eating raw or undercooked meat (particularly mince meat, mutton and pork), and if they own or take care of a cat, make sure the litter box is changed every day, preferably by a friend or family member.
Salmonellosis
Salmonellosis is a common form of food infection that may result when foods containing Salmonella bacteria are eaten. The bacteria are spread through direct or indirect contact with the intestinal contents or waste of animals, including humans. It is estimated that 1.2 million cases of salmonellosis occur each year in the United States. Salmonella bacteria do not grow at refrigerator or freezer temperatures and are easily destroyed by heating foods to 165 degrees F.
Symptoms of salmonellosis include headache, diarrhea, abdominal pain, nausea, chills, fever and vomiting; these usually appear within 12 to 72 hours after eating the contaminated food. Foods most often involved include raw (unpasteurized) milk and raw milk products, raw or undercooked meat and poultry, raw or undercooked eggs, raw sprouts (alfalfa, clover, radish, broccoli), salads (including chicken, tuna, potato), and cream desserts and fillings.
Pregnant women are not at an increased risk for getting salmonellosis; however, one type of Salmonella bacteria, called Salmonella typhi may be passed to the fetus. S. typhi is rare in the United States, but if transmitted to the fetus, can cause abortion, stillbirth or premature labor.
To avoid infection from Salmonella bacteria, pregnant women should follow general safe food handling practices, including washing hands often with hot, soapy water, especially after using the bathroom and before and after handling food. Hands and working surfaces should be thoroughly washed after contact with raw meat, fish, poultry, and foods that will not undergo further cooking. Fresh fruits and vegetables should be rinsed well before eating, and food such as raw milk and raw milk products, raw or undercooked eggs, raw sprouts, raw or undercooked meat and poultry, and unpasteurized fruit juices should be avoided.
Campylobacteriosis
Consuming food or water that contains the bacteria Campylobacter jejuni causes an infection called campylobacteriosis. C. jejuni is found in the intestinal tracts of animals (especially chickens) and in untreated water. It’s a very common cause of diarrhea accompanied by fever in the United States. This organism thrives in a reduced oxygen environment and is inhibited by acid, salt and drying. C. jejuni also is easily destroyed by heat (120 degrees F).
Although pregnant women are not at increased risk of becoming infected with C. jejuni, if they do get sick, the infection may spread to the placenta. Consequences of fetal infection include abortion, stillbirth or preterm delivery. Symptoms usually appear within 2 to 5 days after eating the contaminated food and include fever, stomach cramps, muscle pain, diarrhea, nausea and vomiting. Infection from C. jejuni may be treated with antibiotics.
C. jejuni is most often found in raw (unpasteurized) milk and raw milk products, raw or undercooked meat and poultry, and raw shellfish. To avoid campylobacteriosis, pregnant women are advised to consume only pasteurized milk and milk products and to thoroughly cook meat, poultry and shellfish. Hands, surfaces, cutting boards and utensils that come in contact with raw meat, poultry or fish should be washed well with hot, soapy water.
Preventing Food-borne Illness During Pregnancy
Preventing foodborne illness is always important, but is especially so during pregnancy when the consequences can adversely affect the mother and the unborn child. Listed below are key behaviors important in ensuring the safety of the food you eat.
Practice Personal Hygiene
- Always wash hands well with soap and warm running water for at least 20 seconds before handling food, after using the toilet, after changing a baby’s diaper, and after touching animals.
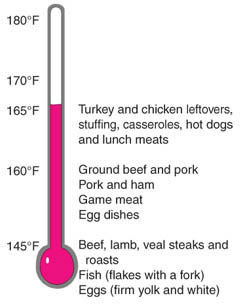 |
Figure 1. Safe endpoint cooking temperatures.
|
Cook Foods Safely
- Use a food thermometer to make sure meat, poultry (including ground meats) and eggs are cooked to safe endpoint temperatures. See Figure 1.
- Use a thermometer to make sure leftovers are reheated to 165 degrees F.
- Always heat hot dogs to steaming hot before eating. Follow the instructions on the package or simmer for at least 5 minutes.
- Heat lunch meats and deli meats to steaming hot before eating. This includes packaged lunch meats and those purchased at the deli. You can use a microwave, oven or grill. If you prefer lunch meats cold, they can be heated and then cooled before eating.
- Cook shellfish until the shell opens and the flesh is fully cooked; cook fish until flesh is firm and flakes easily with a fork or to 145 degrees F.
Avoid Cross-Contamination
- Wash knives, cutting boards and food preparation areas with hot, soapy water after touching raw poultry, meat and seafood.
- As an added precaution, sanitize cutting boards and countertops by rinsing them in a solution made of 1 tablespoon liquid chlorine bleach per gallon of water.
- Wash hands with soap and warm running water after handling raw foods.
- Wash fresh produce well. Rinse fruits and vegetables, and scrub firm-skinned produce, under running tap water, including those with skins and rinds that are not eaten. Pat dry with paper towels.
- Keep cooked and ready-to-eat foods separate from raw meat, poultry, seafood and their juices.
Keep Foods at Safe Temperatures
- Store all perishable foods at or below 40 degrees F. Use a refrigerator thermometer to make sure your refrigerator is between 35 to 40
degrees F. - Store eggs and other perishable foods in the refrigerator.
- Use perishable foods that are precooked or ready-to-eat as soon as possible. If the food cannot be eaten within 4 days, it is best to freeze or discard it.
Avoid Foods from Unsafe Sources
Because pregnant women are at high risk for infection from the pathogens discussed above, they are advised to avoid foods that may be contaminated with these harmful pathogens. See Table 1.
| Table 1. Use the following guide to help choose safe foods during pregnancy, while avoiding foods from unsafe sources. | |
| Instead of… | Choose |
| Cold hot dogs, deli meats and luncheon meats | Hot dogs, luncheon meats and deli meats reheated to steaming hot or 165F |
| Raw or undercooked meat and poultry | Fully cooked meat and poultry |
| Raw or undercooked seafood | Fully cooked seafood |
| Refrigerated smoked fish and precooked seafood such as shrimp, crab and deli seafood salads | Tuna, salmon and crab meat in cans or pouches |
| Refrigerated pâtés and meat spreads | Canned or shelf stable pâtés and meat spreads |
| Raw sprouts and unwashed fruits or vegetables, including lettuce/salads | Cooked sprouts; Well washed fresh vegetables, including salads; Cooked vegetables |
| Soft cheeses made from raw milk such as Feta, Brie, Camembert, blue-veined cheeses, queso fresco, queso blanco and Panela | Hard cheeses, processed cheeses, cream cheese, cottage cheese, mozzarella, and soft cheeses made from pasteurized milk |
| Raw or undercooked eggs | Eggs that are cooked until the white and yolk are firm |
| Raw (unpasteurized) milk and milk products | Pasteurized milk and milk products |
| Unpasteurized juice (May be called “fresh squeezed” or “chilled”) | Frozen concentrate, canned juices and refrigerated juices that are labeled as pasteurized |
References
| For additional safe food handling guidelines, please see Colorado State University Extension fact sheet 9.300, Bacterial Foodborne Illness. |
FSIS-USDA. 2010. Protect your Baby and Yourself from Listeriosis. Available at: https://seafood.oregonstate.edu/sites/agscid7/files/snic/protect-your-baby-and-yourself-from-listeriosis.pdf
Jackson, K.A., Iwamoto, M., Swerdlow, D. 2010. Pregnancy-associated listeriosis. Epidemiol. Infection. 138:1503-1509.
Smith J. L. 1999. Food borne Infections during Pregnancy. J. Food Protection. 62: 818-829.
Smith J. L. 1997. Long-Term Consequences of Food-borne Toxoplasmosis: Effects on the Unborn, the Immunocompromised, the Elderly, and the Immunocompetent. J. Food Protection. 60:1595-1611.
USDA/FDA. 2011. Food Safety for Pregnant Women. https://www.fda.gov/food/people-risk-foodborne-illness/food-safety-pregnant-women-and-their-unborn-babies
* J. Dean, former graduate student, department of food science and human nutrition; P. Kendall, Colorado State
University, associate dean for research, food science and human nutrition. 5/04. Revised 8/12.
Colorado State University, U.S. Department of Agriculture, and Colorado counties cooperating. Extension programs are available to all without discrimination. No endorsement of products mentioned is intended nor is criticism implied of products not mentioned.
Go to top of this page.





